
The Bigger Picture: Stop Blaming Your Pelvic Floor
The function of our pelvic floor muscles is highly influenced by our entire kinetic chain. Here's a look at how.
Ya know, the pelvic floor muscles really get some bad press. Despite their vital role in protecting and supporting your bladder, bowel, reproductive organs, and more, the narrative often revolves around their supposed weakness…
“I am dealing with urinary incontinence because my pelvic floor muscles are weak”
“I have pelvic organ prolapse because my pelvic floor muscles are weak”
“My back pain isn’t going away because my pelvic floor muscles are weak”
“I don’t enjoy sex anymore because my pelvic floor muscles are weak”
(If I may interject- this is important: The word “weak” is wildly misunderstood and does not accurately capture the complexity of pelvic floor function. When we talk about the pelvic floor muscles, loss or limitation of function does not always mean these specific muscles lack strength. They just might be too freakin’ strong (tight) and that’s what causing the problem. We need functional pelvic floor muscles and conventional definitions of “weakness” or “strength” don't necessarily equate to functionality.)
Now, if we accept that pelvic floor disorders are the consequence of weak pelvic floor muscles, the logical approach would be to focus on strengthening them. But it's not as simple as diving headfirst into kegels, even though kegels are pelvic floor-specific. Instead, we have to ask ourselves what else is going on. The key is to understand what might be limiting the function of these muscles.
For example, consider someone with nagging knee pain. They might attribute this pain to quadriceps weakness. Jumping straight into knee extension exercises to specifically strengthen the quads might seem like a logical solution. But we actually need to step back and identify what could be limiting the function of the quads. This issue could very likely stem from limited ankle and hip mobility and weak glutes. Therefore, the appropriate approach would be to address these foundational elements to set up the quads for success.
Finding the right exercise prescription to heal your pelvic floor requires a look at the bigger picture- the whole body. The pelvic floor muscles are interconnected with numerous other parts of our body (even our brain, more on that here) through nerves and connective tissue. The reality is that there are countless potential explanations for what is causing perceived pelvic floor “weakness”.
Let’s explore 5 components of the kinetic chain, NOT your pelvic floor muscles, that might be contributing to your pelvic floor predicament. Keep in mind; this list isn't exhaustive but offers insight into the interconnected nature of our bodily functions. I believe you deserve some specifics here, so I will attempt to be detailed without overwhelming you… we’ll call this “cautiously informative”.
Hip External Rotation:
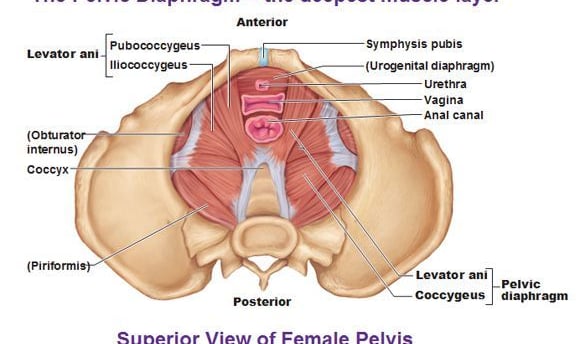
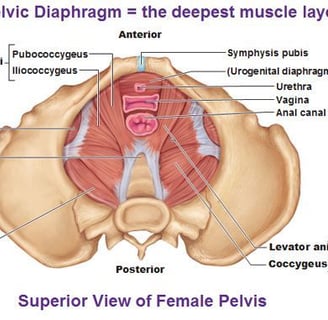
We’ll start with the obturator internus. This muscle’s primary action is hip external rotation- it’s a neighbor to those pelvic floor muscles, yet it can affect your urine and bowel movements. The contribution of hip joint motion to your ability to poop or pee can be explained by the contact between the obturator internus and levator ani (the largest pelvic floor muscle). This connection suggests that movement and strength of the obturator internus contribute to the foundation for the function of the levator ani and provide support to the pelvic floor through the obturator fascia.
Pelvis Position/Pelvic Angle:
While your pelvic floor muscles attach to the pelvis, about a billion (exaggeration) other muscles/attachments dictate pelvis position and angle. Typically, as a pregnancy progresses two things happen to the pelvis: pregnancy-related hormones create more ligament elasticity allowing the pelvis to widen (I’m sure you noticed) and with all that weight added to the front of your body the pelvis tilts forward (anterior pelvic tilt). This increases the possibility of distorted alignment... and misalignment contributes to pelvic girdle pain, back pain, urethra dysfunction and stress urinary incontinence.
Respiratory Diaphragm Function:
Yes, the diaphragm, that big ol’ breathing muscle. There are a lot of different ways that the function of your diaphragm can affect your pelvic floor. Your diaphragm and pelvic floor work in synchrony. As you inhale your diaphragm moves down as does your pelvic floor, providing length to the pelvic floor muscles which helps in maintaining their elasticity- we like ‘em “bouncy”. Stiffness in the diaphragm often translates to stiff pelvic floor muscles, potentially causing various pelvic floor disorders.
Rib Cage Mobility:
Diaphragm function and rib cage mobility go hand-in-hand. Healthy, functional breathing requires a 360-degree expansion of the rib cage to manage abdominal pressure, so our rib cage should be able to expand both laterally and posteriorly. Poor pressure management can increase stress on our pelvic floor, making it harder for these muscles to heal after pregnancy/childbirth.
Foot Health:
The nerves that end in your feet originate from your sciatic nerve. I’m sure many of you have dealt with “sciatica”- that annoying nerve pain that runs down your leg at the least convenient time. Well, the roots of the sciatic nerve begin at the lower lumbar spine and sacrum, run down the back of your thighs, and into the sides of your lower legs and feet. Because of all these nerve endings, your feet contribute to the function of your somatic motor control- so your feet are responsible for important sensory feedback and coordination. They are your foundation! How your feet function will directly affect the way the rest of your kinetic chain functions. You can see how your foot health influences your pelvic floor.
These 5 points barely scratch the surface. If you are experiencing pelvic floor dysfunction, this gives you a peek at why your pelvic floor muscles might not solely be at fault. Understanding these components outside the pelvic floor muscle realm can offer valuable insights into addressing pelvic floor concerns comprehensively.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10008353/
https://www.jospt.org/doi/pdf/10.2519/jospt.2010.3025
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6799872/
https://www.ncbi.nlm.nih.gov/books/NBK537292/
